CHW Project Overview
Acknowledgements
ABCD would like to thank the following individuals for their essential contributions to this project:
Advisory Council Members:
Sharon George, LSWA, Certified CHW,
Anna Thomas, LSWA, CCHW
Amy Oliveira, CCHW
Andrea Mitchell, CCHW
Tia Sommerville, CCHW
Yaminette Diaz-Linhart, MSW,PhD, Consultant
Jennifer Valenzuela, MSW, MPH, Health Leads
Rebekah Gerwitz, National Association of Social Workers, MA Chapter
Geoff Wilkenson, MSW, Boston University School of Social Work
Trainers:
Jules Patigian, LMHC- lead curriculum author, and trainer of trainers, SameBoat Consulting
Areliz Barbosa, CCHW
Devorath Ruiz, MSW, LICSW
Deb Goldfarb, MSW, LICSW
Daniel L. Do, MSW, MPH, Doctoral candidate
ABCD Staff:
Jessica Aguilera-Steinert, MSW, LICSW, Director Health Services, Consultant, lead program director
Nancy Paladino, RD, Director Health Services, program director
Erin McSweeney, Training and Technical Assistance Coordinator, editor
Ellisa Dockstader, Community Prevention Manager, coordinator
Olivia Lopes, MSW intern
Margaret Fryerwood, MPH, Training Coordinator
Evaluators:
Linda Sprauge Martinez, PhD
Melanie Rocco, MSW, MPH
Toolbox Introduction and Background
The purpose of the CHW Behavioral Health Integration toolkit is to share training materials and research-based insights that might benefit employers of CHWs and other health professionals, training organizations, payers, community health worker programs, and policy makers. It will assist organizational planners, program managers, supervisors and other stakeholders in successfully integrating CHWs into the behavioral health services at their health setting.
A) Intro to ABCD and Health Services: ABCD is a non profit community action agency that each year provides 100,000 low income residents in the Greater Boston region with tools and resources needed to transition from poverty to stability and stability to success. The ABCD Health Services Department is committed to keeping low income residents and communities healthy through public health promotion and wellness programs, including Title X family planning, and by training health professionals in the Training Institute. Our rich community partnerships contribute to the success of our efforts
B) Funding overview: ABCD received 3 years of grant funding from Massachusetts General Hospital’s Center for Health Care Improvement grant program. This grant funding was designed with the goal of “increasing access to behavioral health services through community health workers and workforce development. This funding was made available by the Massachusetts Determination of Need (DoN) process regulating community investment as hospital capital improvement projects are approved. “ Mass General Awards
ABCD applied under the Community Health Worker and Behavioral Health arm and designed this unique training program.
C) Project team: This project was a labor of love and had a large group of professionals involved in the design, implementation and evaluation of the program. Early in the planning phase, the ABCD program team created an Advisory Council which included professionals working in behavioral health or community health including representatives from national and local organizations including Health Leads, National Association of Social Workers, MA Chapter, Massachusetts Association of CHWs, the Boston University of School of Social Work’s Center for innovation in Social Work and Health, as well as individuals who have decades of experience managing CHW programs and working as CHWs in health care. CHWs were the most important members of the Council and made up 50% of the initial advisory team. In addition, the program team recruited 6 social workers and CHWs to be trained as co- trainers for the behavioral health integration training for CHWs and their supervisors. Finally, ABCD contracted with Linda Sprague Martinez, PhD., to conduct a qualitative and quantitative evaluation.
Project Overview
Project summary: In health care settings such as community health centers (CHCs) or hospital- based primary care, Community Health Workers (CHWs) support, advocate for, and accompany patients with chronic diseases and behavioral health (BH) comorbidities. However, efforts to involve CHWs in delivering evidence-based mental health interventions to under-served communities need to be improved by enhancing access to and understanding of the BH conditions and organizational systems. Additionally, social workers and other BH clinicians need ways to understand and leverage the unique skills and identities of CHWs to best serve their common patients.
In some public health settings, there is discomfort and mistrust between BH clinicians and CHWs. These professionals are similarly grounded in social justice values and serve as advocates for their patients. Overwhelmingly though, the BH clinicians do not come from the communities they serve, nor have personal experience of the racism and oppression that can result in mistrust of BH clinicians. Conversely, CHWs who do come from the communities they serve, and have experienced racism and oppression, are often less trained in the complex clinical components of mental illness and substance use. There is uncertainty by clinicians that CHWs have the ability to appropriately work with clients with mental health challenges. Both BH clinicians and CHWs agree that there needs to be understanding and education of both groups to improve their collaboration to better and more efficiently serve patients.
The CHW Behavioral Health Integration Project (CBIP) combines intensive training for CHWs on mental health and substance use disorders (SUD) most commonly presented in primary care, skill building around BH service navigation, and data and analysis about how race plays a significant role in behavioral health outcomes. The CHW Supervisor training focuses on an overview of what the CHWs are trained on and teaches skills in Supportive Supervision also known as Reflective and Clinical Supervision commonly practiced by mental health clinicians who supervise. More helpful information on CHW Supervision can be accessed here: Six Tips for CHW Supervision Success – MHP Salud and here Supervision Strategies and Community Health Worker Effectiveness in Health Care Settings – National Academy of Medicine.
The Supervisor training also addresses racial equity issues in behavioral health and in supervision dynamics, as well as important integration strategies to increase effective collaboration between Behavioral Health clinicians and CHWs in health settings.
This technical assistance toolkit includes recommendations and tools to help health center and hospital leadership enhance their BH services through improved integration of CHWs into their teams while recognizing, rather than supplanting, the skill, knowledge and training of BH clinicians. There is room and need for both workforces in the service of patients with complex needs. A recent evaluation of CHWs involved in evidence-based mental health interventions found promising results and encouraged this practice as an opportunity to reduce the mental health disparity gap.
Critical need for CHW training in Behavioral Health: Depression, anxiety, drug and alcohol misuse are at epidemic levels in many urban and rural areas in the US. According to the Boston and North Suffolk CHNA surveys, MassGeneral 2020 CHIP mental health and substance use were in the top three most reported concerns that affect the health of the members of these communities.
In the 2017 MDPH report on Behavioral Health and Community Health Worker Training, behavioral health training appropriate for CHWs was limited in MA. It is also noted there is a greater need for increased availability and a wider variety of BH trainings as identified by CHWs, their managers, and training program directors. In fact, mental health and substance use training were two topics identified by CHWs that were the most needed. In the past few years, there has been a growing recognition and hiring of CHWs among Accountable Care Organizations, Community Partners, and health plans as members of both medical and behavioral health care teams. The need for CHWs with improved BH training and related skills is only growing in Massachusetts.
Increasingly, CHWs are being assigned to work with people with complex medical and behavioral health conditions. CHWs are hired specifically because of their similar lived experiences and ability to identify and build trust with our most vulnerable residents. They are well positioned to help ascertain behavioral health needs and help clients navigate the complex medical and behavioral health systems. Many studies indicate a relationship between experiences of racism in the US and negative mental health outcomes. The trainings provided participants with the knowledge and tools needed to further break down the stigmas and barriers associated with mental health for Black, Latinx and immigrant communities.
A total of 88 CHWs initiated the baseline evaluation survey. Of those who enrolled, the vast majority had patients in their caseloads with behavioral health conditions; and nearly half of participants reported that more than 51% of their caseload was composed of patients with identified behavioral health needs.
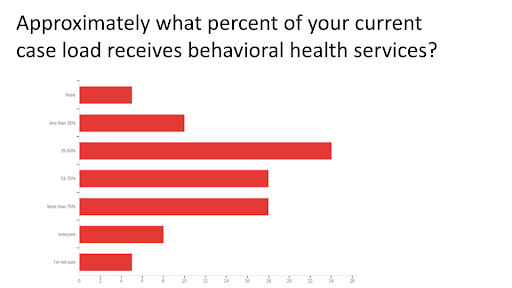
Almost all participants reported making behavioral health referrals within their agency and nearly half reported frequent agency referrals. This pattern was consistent for referrals outside of the agency.
___
NEXT > CHW TRAINING MODEL
